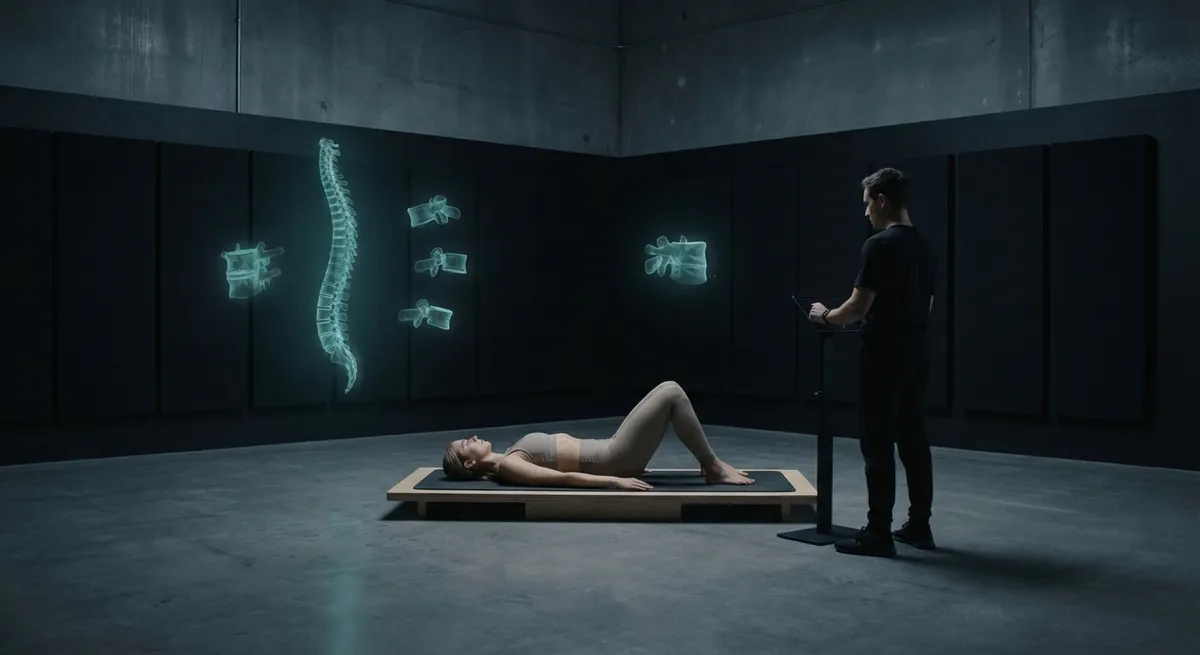
Backs that bear the weight of demanding lives need more than generic advice and occasional stretching. They require movement that is curated, not improvised—exercise chosen with the same discernment you would bring to a tailored suit or a well-designed workspace. Exercise therapy, when approached as precision medicine rather than “working out,” becomes one of the most refined tools for preserving spinal health and reclaiming comfort.
This is not about athletic performance or aesthetics. It is about teaching your spine to move intelligently, distributing effort with elegance instead of strain. Below are five exclusive insights that elevate exercise therapy from a chore into a strategic, high-yield investment in your back.
The Spine Is an Orchestra, Not a Soloist
Most people treat back pain as if the spine exists in isolation: stretch the back, strengthen the back, “fix” the back. In reality, your spine behaves more like the conductor of an orchestra—reliant on the precision and timing of the muscles around the hips, pelvis, ribcage, and even feet.
When the deep stabilizing muscles of the trunk (such as the multifidus and transverse abdominis) are undertrained, louder “musicians” step in—the large global muscles that were never meant to handle fine control. This compensation may look like strength, but it often produces rigidity, stiffness, and pain over time.
Sophisticated exercise therapy trains the entire ensemble: gluteal strength to reduce load through the lumbar spine, hip mobility to allow graceful rotation, thoracic extension to prevent the lower back from doing the job of the mid-spine. Reform-oriented movement, such as carefully designed Pilates or clinical-strength programs, focuses on this integrated orchestration rather than on one area in isolation.
For discerning backs, the goal is not maximal effort but balanced recruitment—each muscle doing exactly enough, not too much. The result is a spine that moves with quiet competence rather than constant firefighting.
Micro-Dosing Movement: The New Standard of Spinal Luxury
Traditional thinking prizes the single, dedicated workout: 45–60 minutes, a few times per week. For a spine subjected to long hours of sitting, travel, or high-stakes work, that model is quietly outdated.
The more refined strategy is micro-dosing movement—short, precise bouts of exercise woven seamlessly into your day. Think of it as metabolic “maintenance” for the spine: two minutes of guided lumbar mobility between meetings, three slow, controlled squats while your coffee brews, a 5-minute evening sequence targeted to undo your particular postural habits.
This approach respects a critical truth: your spine responds less to what you do occasionally and far more to what you repeat consistently. Digestible movement doses protect you from the “all or nothing” trap—weeks of good intention followed by derailment when life becomes demanding.
Micro-dosing also allows for exceptional tailoring. On days with increased sitting or air travel, you might emphasize hip flexor release and gentle spinal decompression. After strength training or long walks, you might prioritize controlled core activation and nuanced rotation. Over time, this repeated, intentional exposure teaches your spine that movement is the default, not the exception.
Precision Strength: Why “Core Work” Is Often Too Crude
“Core strengthening” is one of the most overused—and misunderstood—phrases in back care. Many routines marketed as core work are, in fact, generic abdominal workouts that can overload the spine rather than support it.
Premium exercise therapy distinguishes between three layers of support:
- **Deep stabilizers** (multifidus, transverse abdominis, pelvic floor, diaphragm): These create subtle, anticipatory tension around the spine before movement even begins.
- **Intermediate stabilizers** (obliques, glute medius, deep hip rotators): These guide and fine-tune your movement.
- **Global movers** (rectus abdominis, erector spinae, big hip muscles): These handle power, not precision.
Refined programs start from the inside out. The work feels understated—gentle bracing while breathing, precise pelvic tilts, carefully aligned dead bugs, or bird-dog variations done with surgical control. The objective is exquisite timing and endurance, not exhaustion.
Only once these deeper layers are reliable do you gradually introduce more complex and loaded patterns (hinges, split squats, loaded carries). This phased approach transforms your spine from reactive and guarded to quietly resilient—even under demanding conditions like travel, long presentations, or extended screen time.
Intelligent Recovery: The Missing Half of Exercise Therapy
Elite recovery is not a luxury reserved for athletes; it is a necessity for any spine placed under repetitive load—whether from training, sitting, or stress.
Thoughtful recovery for back health involves three key elements:
**Strategic down-regulation**
Stress and spinal tension are inseparable. Exercise that supports the back includes intentional exit strategies: slow nasal breathing after sessions, brief restorative positions (such as supported child’s pose or 90/90 hip and knee flexion), or guided mobility focused on calming rather than pushing.
**Load cycling rather than random intensity**
A sophisticated program alternates heavier, more demanding days with lighter, restorative ones. For example, a week might combine one day of strength emphasis, one day of low-impact conditioning (such as walking or cycling), and one or two short therapeutic mobility sequences. This cadence protects the spine from the overzealous “new routine” that flares pain and erodes consistency.
**Sleep and timing as active components of therapy**
Exercise that irritates your back late in the evening may blunt recovery. Gentle mobility and breath-focused routines before bed can improve both pain modulation and sleep quality, indirectly supporting spinal healing. It is not simply *what* you do, but *when* and *how* it interfaces with your body’s repair cycles.
Recovery, approached this way, is not passive rest; it is an active, curated process that allows the spine to absorb the benefits of exercise instead of merely surviving it.
Personal Baselines: Building Your Private Back-Health Dashboard
Sophisticated back care treats your body as data-rich, not mysterious. The most effective exercise therapy programs are anchored by a few personal metrics—simple, repeatable checks that tell you whether your spine is trending in the right direction.
For example, you might track:
- How easily you can perform a pain-free hip hinge (folding at the hips while keeping a neutral spine).
- Your ability to roll from back to side without bracing or holding your breath.
- How long you can maintain a high-quality side plank on each side.
- Whether you can sit for a set period (e.g., 45 minutes) with minimal discomfort after your weekly routines.
- Morning stiffness duration: how long it takes each day to feel “fully mobile.”
These become your private dashboard—more informative than any single pain score. If a well-designed exercise block improves these metrics over weeks, you know you are building capacity, even if discomfort has not vanished entirely. If they worsen, that is early feedback that your load, intensity, or movement selection needs refinement.
This data-driven, yet personal approach transforms exercise therapy from guesswork into an ongoing dialogue with your spine. The process becomes less about chasing relief in the moment and more about steadily upgrading the way your back behaves under real-world demands.
Conclusion
In an age of constant sitting, digital strain, and accelerated schedules, the spine is both remarkably forgiving and quietly exacting. It responds not to extremes, but to thoughtful, well-distributed effort—movement that respects its complexity rather than overpowering it.
Exercise therapy, when practiced as precision medicine, is not about punishing workouts or rigid regimens. It is about orchestrated strength, curated micro-movements, deep stabilizing intelligence, deliberate recovery, and personal metrics that tell you, clearly, when you are on the right path.
For those who require their back to perform without drama—through long flights, intensive workdays, and ambitious personal lives—this level of refinement is not indulgent. It is the new standard of responsible, high-level back care.
Sources
- [National Institutes of Health – Core Stabilization Exercise Principles](https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3812831/) – Explores the role of deep trunk muscles and stabilization exercises in managing low back pain
- [Harvard Health Publishing – Protecting Your Back](https://www.health.harvard.edu/pain/protecting-your-back) – Overview of evidence-based strategies including exercise and movement for back health
- [Mayo Clinic – Back Pain: Self-Management](https://www.mayoclinic.org/diseases-conditions/back-pain/in-depth/back-pain/art-20043921) – Discusses lifestyle, exercise, and practical management approaches for back pain
- [Cleveland Clinic – Physical Therapy for Low Back Pain](https://my.clevelandclinic.org/health/treatments/17296-physical-therapy-for-low-back-pain) – Details how targeted exercise and physical therapy support recovery and prevention
- [NHS (UK) – Exercises for Back Pain](https://www.nhs.uk/live-well/exercise/exercises-to-help-back-pain/) – Provides clinically recommended exercises and guidance for maintaining spinal mobility and strength
Key Takeaway
The most important thing to remember from this article is that this information can change how you think about Exercise Therapy.